The process of making vaccines for parasites is extremely challenging – but scientists might be on the cusp of major breakthroughs.
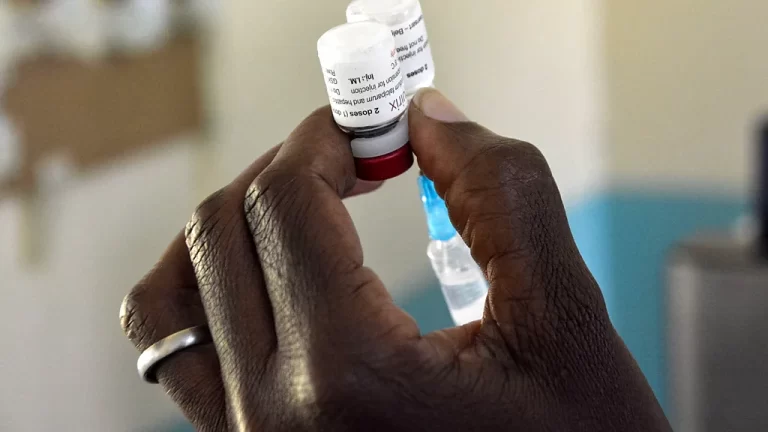
There was much celebration in January, when Cameroon became the first country in the world to roll out routine vaccination against malaria. In February, Burkina Faso followed suit.
“Control of malaria has not been going in a good direction, for a lot of different reasons,” explains Kate O'Brien, who directs the department of immunisation, vaccines and biologicals at the World Health Organization (WHO). Malaria cases are rising, and roughly 600,000 people die of malaria each year. Factors include climate change, conflict, the lingering effects of Covid-19 on health systems, and the tenacious adaptability of malaria-carrying mosquitoes. This has meant that the stalwarts of malaria prevention – insecticides sprayed indoors and bed nets treated with insecticides – are losing some of their punch.
Mass malaria vaccination adds one more tool to this package, and one that takes a completely different approach, says O'Brien. “Coming in with an immune-based approach is a very historic and important addition,” she says. In 2019 the RTS,S vaccine against malaria began pilots in Ghana, Kenya and Malawi, and in 2021 the WHO recommended it for use in children. The RTS,S vaccine was followed by the R21 vaccine.
Yet a related milestone has gone less heralded. RTS,S was the first-ever vaccine against a parasitic disease. While diseases caused by parasites are numerous and varied, as a group they are understudied and solutions are underfunded. Most of the neglected tropical diseases, including leishmaniasis and Chagas disease, are parasitic diseases, according to the WHO.
There wasn't necessarily a concerted effort to make the malaria vaccine the first antiparasitic vaccine. But it's perhaps unsurprising that it ultimately was, as the high death toll exacted by malaria has led to more attention to developing vaccines for malaria than for other parasitic illnesses (though still not as much as for vaccines affecting wealthy populations, such as Covid-19).
This high mortality rate from malaria makes it a bit of an outlier among parasitic illnesses. Overall, “the death rate from parasitic diseases…is relatively low compared to some other infectious diseases”, O'Brien says. The effects can be disabling and devastating, but not necessarily fatal. Because of this, and because parasitic diseases often are limited to specific parts of low- and middle-income countries, they haven't been prioritised by conventional vaccine developers.
Peter Hotez is not a conventional vaccine developer. The professor at the Baylor College of Medicine in Houston, who also co-directs the Texas Children's Hospital Center for Vaccine Development, worked with colleagues to create a late-entrant Covid-19 vaccine that was transferred, free of patent, to vaccine manufacturers in India and Indonesia. At least 100 million doses of the Indian version, Corbevax, have been supplied at approximately $3 (£2.38) per dose. The developers chose an inexpensive vaccine technology: essentially producing a protein in yeast through microbial fermentation. The team are hoping to apply some of the lessons learned from this experience to their work on antiparasitic vaccines, he says.
Parasites pose many challenges to vaccine developers
Of course, massive energy and financial resources were poured into the creation of multiple Covid-19 vaccines. But this isn't the only reason those vaccines appeared relatively quickly. “There's no question that parasites are far more complicated targets than viruses,” Hotez says. “Compared to a coronavirus vaccine, which is about the lowest hanging fruit there is…it's not as straightforward with something like a hookworm vaccine,” he says.
One technical challenge of working with parasites is their enormous genetic diversity, which can make it difficult to target a specific species or strain
A hookworm is a parasitic worm that feeds on intestinal blood, leading to anaemia and nutrient deficiencies. “Think of it as an animal. You're making a vaccine against an animal,” Hotez says.
Almost all existing vaccines work against bacteria and viruses, there are currently no vaccines against fungi anywhere in the world, and there is just one type of vaccine – the anti-malarial one – against parasites. Parasites often have sophisticated ways of evading a host's immune system. They adapt to their hosts during complex life cycles, involving several developmental stages. “Each one of those stages, either in an animal or a human host, has different proteins that are expressed in the different life stages. And that makes it more complicated to identify what the targets could be of the parasite for development of a vaccine,” says O'Brien.
This life cycle complexity is one of the reasons that parasites aren't always easy to culture in a laboratory. In other words, it can be tough to simply produce more of them under controlled conditions, at the right stage of development, for research purposes. Possibilities including cultivating parasites in research animals or in a laboratory, rather than in their usual hosts.
Epidemiologist Miriam Tendler coordinates the Sm14 Anti Helminth Vaccine Initiative at the Oswaldo Cruz Foundation (Fiocruz) in Rio de Janeiro. In particular, the team studies parasitic worms, including schistosomes, which affect some 240 million people globally and currently have limited treatment options. Schistosomes are just one type of helminths, a group of worms (including hookworms) which commonly cause chronic disease in lower-income countries.
One technical challenge of working with parasites is their enormous genetic diversity, which can make it difficult to target a specific species or strain. Tendler and her colleagues found a workaround by identifying a common key component in many helminth species. They found that the protein Sm14 is present in multiple species of helminths that cause disease in humans and livestock, not just schistosomiasis.
Tendler and her team have now developed a vaccine against schistosomiasis, and it has completed some Phase 2 clinical trials. She recalls that in the early days of developing this vaccine, she and her team had to extract the protein from adult worms. But after identifying, sequencing and cloning this recombinant protein, they can now produce litres of it in fermenters.
Because several types of worms produce the protein Sm14, the schistosomiasis vaccine that the team is developing may also work against several other diseases caused by different helminth species, says Tendler. Thus, a single type of vaccine, in different formulations, could help protect children against schistosomiasis, cattle against fascioliasis, and even pet dogs against heartworm.
Financing antiparasitic vaccines
Tendler's team has been working in parallel on the human and non-human versions of the Sm14 vaccine, and insights from this joint research have helped them to reach the current level of development. The human schistosomiasis vaccine is currently in clinical trials in Senegal, and Tendler expects it to finally be available within three years. “It's a big thrill,” she says, of her team's success.
This parallel vaccine development in humans and animals may have also helped to move forward conversations about the critical need for vaccines to combat parasitic worms, which will continue to reinfect people who live in affected areas. “The impact on quality of life for humans, mainly children, is very, very high,” Tendler says.
But while schistosomiasis and other diseases caused by helminths mostly affect people in poorer countries, from a livestock standpoint, helminths harm the livelihoods of people in richer countries as well – creating more of a market incentive. The potential veterinary vaccine against helminths has been licensed to FABP Biotech, a private company spun out of Fiocruz, while the human vaccine is being financed primarily by the Brazilian government.
The latter will be a “humanitarian vaccine”, Tendler emphasises. The plan is for Fiocruz's Institute of Technology on Immunobiologicals (Bio-Manguinhos) to produce it at less than $1 (£0.79) a dose, with further cost reductions possible as production scales up gradually to eventually reach the target of one billion doses. There will be a limitation on the profit margin.
The hookworm vaccine is also likely to be manufactured outside of the major multinational pharmaceutical companies. Hotez expects it to be produced by a member of the Developing Countries Vaccine Manufacturers Network, which includes Brazil's Bio-Manguinhos as well as manufacturers in China, India, South Africa and other countries. “The problem is our technology to make vaccines has outpaced our political, social, economic and legal frameworks to get them actually scaled and produced,” says Hotez.
The future of vaccines for parasitic diseases
Although antiparasitic vaccines are badly needed, they shouldn't be treated as silver bullets, says O'Brien. “There is no malaria intervention that has perfect performance. We have a toolbox of prevention measures,” she says. As a tool to reduce the likelihood and severity of infection, the malaria vaccine is an addition to, rather than a replacement of, the other measures in the toolbox. Importantly, communities where the RTS,S vaccine has been piloted have not reduced their use of bed nets.
These historic antiparasitic vaccines are expected to be followed by others targeting the same diseases, which could improve their speed of development and their efficacy. Researchers recently reported an average 78% efficacy rate for the R21 malaria vaccine (which they called “high efficacy”). This was based on trials in five to 17-month-olds in Burkina Faso, Kenya, Mali and Tanzania.
For context, “vaccines that give 97% protection like measles are in some ways the exception rather than the rule,” Hotez says.
“We shouldn't focus our attention quite as much as we do on the efficacy,” says O'Brien. While it's an important number, she believes that what matters more is the impact, which depends on the access to a vaccine and its effect on the burden of disease.
There are also some broader benefits to the series of breakthroughs with malaria vaccines. “The success of this vaccine instils hope for a similar victory for an equally challenging pathogen [helminths] which causes a significant amount of morbidity globally, though it receives much less attention and fewer resources,” says Jeffrey Bethony, a microbiologist at George Washington University in Washington, DC.
Just as similar vaccine technologies may be used across HIV and coronavirus vaccines, the strategies used for malaria vaccines are useful in regard to other types of blood-feeding parasites, says Bethony. “A rising tide lifts all boats here,” he says.
Hotez hopes that the precedent setting will extend not only to the technical aspects of developing vaccines for neglected tropical diseases, but also to getting those vaccines where they're needed. “One of the more interesting parts of this is also one of the more terrifying parts,” Hotez says. While “it's an amazing feeling to know that you're pioneering this very innovative model for providing access to innovation to the poorest people on the planet, it's also terrifying because there's no road map,”
— CutC by bbc.com